The church has always been called to lead in truth, compassion, and purpose. Its highest mission has never changed — to honor God for who He is through worship and praise, to present the Gospel of Jesus Christ, and to advance His Kingdom on earth.
In every generation, God moves by His Spirit upon the souls of men and women — directing the actions, decisions, and expressions of their bodies. The body is not secondary to God’s plan; it is the vessel through which His Spirit accomplishes His will on earth.
But in the modern church, this truth has been largely forgotten.
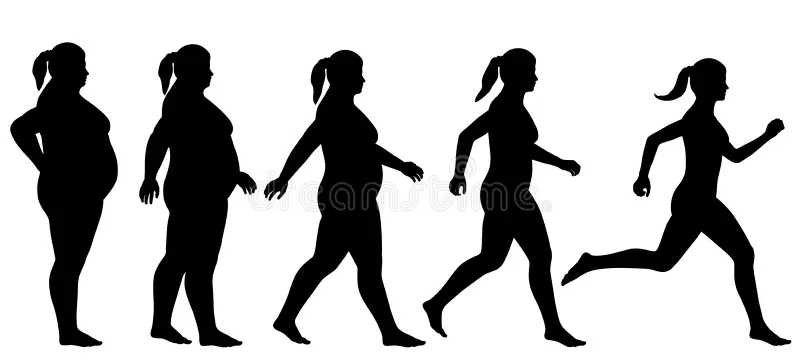
We have cultivated deep spiritual awareness yet allowed physical stewardship to fade into neglect. The result is a generation of believers spiritually alive but physically depleted — unable to serve, endure, or lead with the energy and health God intended.
Created with Intent — Flesh and Spirit Together
When God formed man, He already had a heavenly family — angels, spiritual beings who existed in His presence. But He desired something different — an earthly family that would bear His image in a physical world.
“Then the Lord God formed man from the dust of the ground and breathed into his nostrils the breath of life.” — Genesis 2:7
He made us flesh and blood on purpose. He didn’t make a mistake by giving us physical bodies. He called them good.
Our physical form is not a burden to escape — it is a platform for obedience. We are designed to co-labor with God in the administration of His creation.
That means what we do with our bodies — our energy, our movement, our health — matters deeply to Him.
The Modern Church’s Blind Spot
In the 21st century, the Church preaches faith, hope, and love, yet often neglects discipline, stewardship, and embodiment.
We have become technology-dependent, sedentary, and overfed.
The physical health of the body of Christ no longer reflects the vitality of its spirit.
We cannot ignore that:
- Over 70% of American adults are overweight or obese.
- Physical inactivity is now one of the leading risk factors for chronic disease worldwide.
- Depression and anxiety are rising at the same rate as physical inactivity.
And yet, few pulpits address this reality.
We pray for healing — but ignore the habits that produce sickness.
We teach spiritual discipline — but avoid physical discipline.
We speak of surrendering all to God — yet treat our bodies as exceptions.
Dependency, Not Independence
The aim is not to glorify the body or pursue the “body beautiful.”
This is not about vanity, appearance, or competition.
This is about dependence on God in all areas, including the stewardship of the physical frame He gave us.
True stewardship of the body begins with humility — acknowledging that:
- God owns it.
- The Spirit inhabits it.
- Our actions reflect our dependence on Him.
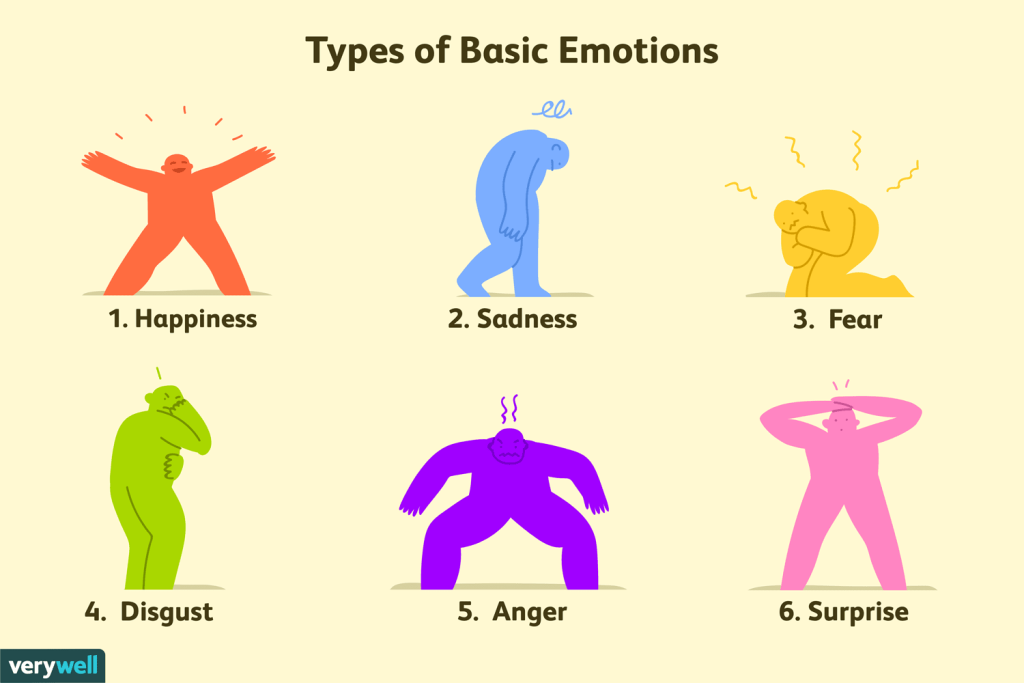
When the Spirit directs the soul, and the soul commands the body, we function as whole people — spirit, soul, and body in alignment.
That is biblical order. Anything else is disorder — and the modern church is suffering from it.
A Theology of Movement
Movement was part of God’s design long before gyms existed.
From the first garden, humanity was meant to walk, work, and cultivate. The command was active:
“The Lord God took the man and put him in the garden of Eden to work it and keep it.” — Genesis 2:15
Work and worship were never meant to be separate.
When we move, train, and steward our strength, we are not performing for vanity — we are worshiping through obedience.
We are honoring the God who designed muscle, energy, and endurance as instruments of purpose.
Why the Church Must Reclaim Physical Stewardship
- The Body Is God’s Instrument of Mission.
The hands that serve, the feet that go, the lungs that sing — all are physical vessels of Kingdom work. Weak bodies limit strong callings. - Neglect Breeds Disconnection.
Physical decline often mirrors spiritual apathy. When we lose discipline in one area, it affects the others. - The Next Generation Is Watching.
Our children are being raised in a world of comfort, convenience, and screens. If the Church won’t model physical stewardship, who will? - Stewardship Reflects Honor.
You cannot separate worship from obedience. Caring for your body is an act of honor toward the One who made it.
Restoring the Discipline
To restore the biblical model of health, the Church must teach embodiment as stewardship, not self-worship.
- Integrate movement, nutrition, and rest into discipleship.
- Host classes or gatherings that reconnect faith with physical stewardship.
- Encourage walking groups, corporate fasting, and teaching on bodily discipline.
- Train the congregation to see health as worship, not as a secular pursuit.
These steps reintroduce dependency — not on methods or trends, but on God’s wisdom guiding human action.
The Aruka Perspective
Aruka’s mission has always been to unify what the world separates — spirit, soul, and body.
When one system weakens, all suffer.
The Church must again become the example of integrated health — spiritually vibrant, emotionally grounded, and physically capable of advancing the mission of God on earth.
This isn’t about image — it’s about integrity.
It’s about being fully alive to serve a living God.
Final Thought
The Church’s greatest calling remains unchanged: to glorify God and make Him known.
But in this modern age, we must recognize that glorifying God also means honoring how He created us — as physical, embodied beings called to move, work, and steward our strength in service of His purpose.
We were not created to sit and consume.
We were created to move, build, serve, and reflect His image with vitality.
Our bodies are not obstacles to worship — they are instruments of it.
When the Church rediscovers that truth, it will reclaim a missing element of its witness to the world.